Urinary incontinence (UI) is a condition that affects millions of people worldwide, impacting their quality of life and confidence. Traditionally managed through medications, pelvic floor exercises, or invasive surgeries, a non-invasive approach using High-Intensity Focused Electromagnetic (HIFEM®) technology has gained significant attention for its effectiveness and convenience. Dr. Julene B. Samuels presented her findings on the long-term efficacy of the HIFEM procedure at the 40th Annual Meeting of the American Society for Laser Medicine and Surgery. The data highlights promising outcomes, particularly at 6 months and 1-year follow-ups, suggesting the procedure is an excellent option for managing UI.

What is Urinary Incontinence (UI)?
UI refers to the involuntary leakage of urine, a condition that can significantly disrupt daily life. Common types include:
- Stress Incontinence: Leaks caused by physical activity or pressure, such as coughing or exercising.
- Urge Incontinence: A sudden and strong urge to urinate that can result in accidents.
- Mixed Incontinence: A combination of stress and urge incontinence.
UI often results from weakened pelvic floor muscles, typically due to aging, childbirth, or medical conditions.
Understanding HIFEM® Technology
HIFEM® technology is a non-invasive procedure that stimulates the pelvic floor muscles through electromagnetic energy. This causes thousands of supramaximal contractions in each session, strengthening and re-educating the muscles responsible for bladder control.

Key Benefits of HIFEM® for UI
- Non-Invasive: No needles, surgeries, or recovery time.
- Effortless: Unlike Kegel exercises, the technology does the heavy lifting.
- Efficient: Each session lasts only 28 minutes, making it a convenient solution for busy lifestyles.
Study Overview: Measuring Long-Term Efficacy
Dr. Julene B. Samuels analyzed the outcomes of HIFEM treatment in patients with urinary incontinence, focusing on improvements in symptoms, quality of life, and pad usage over 1 year. The study utilized the International Consultation on Incontinence Questionnaire – Short Form (ICIQ-SF) to measure symptom severity and the need for absorbent pads to evaluate practical impact.
ICIQ-SF Score Explained
- A higher score indicates more severe UI symptoms.
- A lower score signifies improvement and better bladder control.
Results at a Glance: 6 Months and 1-Year Follow-Up
Continuous Improvement at 6 Months
Patients showed steady progress, with significant improvements in their ICIQ-SF scores and quality of life.Slight Regression at 1 Year
While most patients maintained improvements, a slight rise in ICIQ-SF scores at the 1-year mark was noted, primarily due to one subject experiencing a complete loss of treatment outcomes.Reduction in Pad Usage
- Baseline: Patients used an average of 3.0 absorbent pads per 24 hours.
- 1 Year: Usage decreased to 1.4 pads per 24 hours, indicating a substantial reduction in leakage severity.
Detailed Findings
ICIQ-SF Score Trends
- Baseline: Patients reported high symptom severity.
- Post-Treatment (Immediately After): Rapid improvements were observed, with reduced urgency and leakage.
- 3-Month Follow-Up (3MFU): Progress continued as patients adapted to stronger pelvic floor muscles.
- 6-Month Follow-Up (6MFU): Marked improvement, with most participants experiencing minimal symptoms.
- 1-Year Follow-Up (1YFU): A slight rise in ICIQ-SF scores was noted, suggesting that some patients may benefit from maintenance treatments.
Maintenance Treatment Implications
The data implies that while the HIFEM procedure is highly effective, certain patients may require booster sessions after 1 year to sustain optimal results.
Impact on Absorbent Pad Usage
One of the most tangible improvements was the reduced reliance on absorbent pads.
- Patients reported feeling more confident and less dependent on pads for daily activities.
- Reduced pad usage also alleviates the financial burden associated with managing UI.
Why HIFEM® Works
HIFEM technology targets the root cause of UI: weakened pelvic floor muscles. Here’s why it’s effective:

- Pelvic Floor Strengthening: Thousands of muscle contractions during treatment restore muscle tone and function.
- Neuromuscular Re-Education: The procedure helps retrain the brain-muscle connection, leading to improved bladder control.
- Non-Invasive Approach: Unlike surgeries, HIFEM avoids complications, downtime, and invasive procedures.
Patient Experience: What to Expect
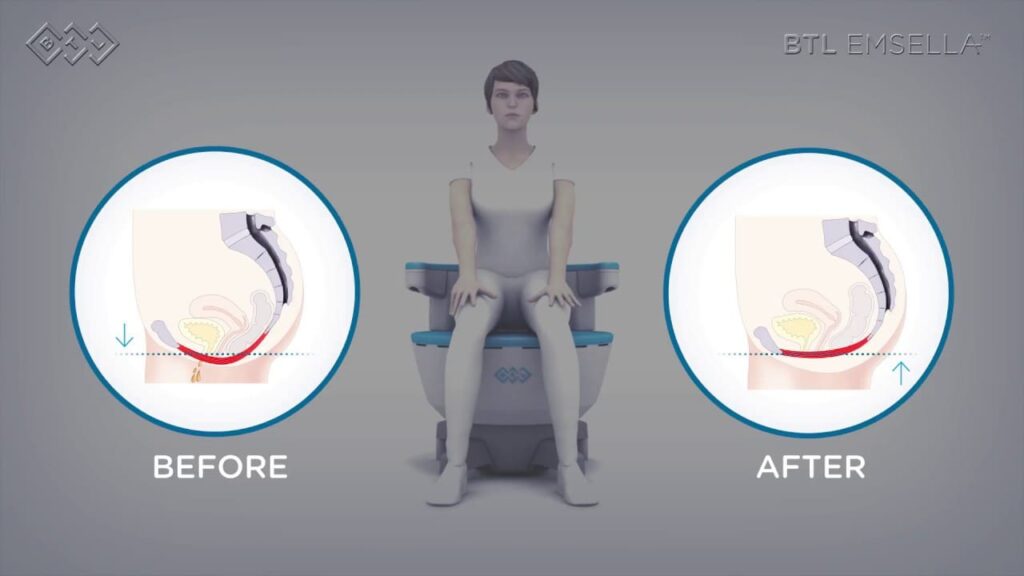
During the Procedure
- Patients sit comfortably while the HIFEM device stimulates their pelvic floor muscles.
- The treatment is painless, with most describing the sensation as a mild pulling or tingling.
After the Procedure
- There’s no downtime; patients can resume normal activities immediately.
- Noticeable improvements often begin after the first few sessions, with full results typically evident by 6 months.
Comparison with Traditional UI Treatments
| Treatment | Invasiveness | Effectiveness | Drawbacks |
|---|---|---|---|
| HIFEM® | Non-Invasive | High | Requires maintenance after 1 year |
| Pelvic Floor Exercises | Non-Invasive | Moderate | Requires discipline and proper form |
| Medications | Non-Invasive | Varies | Potential side effects like dry mouth |
| Surgery | Invasive | High | Risk of complications and recovery |
Real-Life Transformations
Emma, 55
“I had been using pads for years and felt frustrated with my lack of control. After completing my HIFEM sessions, I now use less than one pad a day—and sometimes none at all!”
Linda, 43
“HIFEM gave me my confidence back. I can laugh, run, and live without worrying about leaks. It’s been a game-changer.”
Future of HIFEM Technology
The long-term success of HIFEM in treating UI suggests potential for broader applications:
- Postpartum Recovery: Helping new mothers regain pelvic strength.
- Prostate Health: Expanding its use to address male UI and other pelvic issues.
- Athletic Performance: Strengthening core stability and endurance through pelvic muscle toning.
Conclusion: A Breakthrough in Managing UI
The HIFEM procedure offers a revolutionary, non-invasive approach to treating urinary incontinence. Dr. Julene B. Samuels’ study demonstrates its long-term efficacy, with most patients maintaining significant improvements in bladder control and quality of life up to 1 year.
While slight regressions were observed in some cases, the overall results underscore HIFEM’s potential as a preferred treatment option. Incorporating maintenance sessions could ensure lasting benefits for all patients.
For those seeking a solution to UI without the risks of surgery or the discipline required for exercises, HIFEM offers a promising path to improved confidence and well-being.
FAQs
1. How long do the effects of HIFEM last?
Most patients experience significant improvements for up to 1 year. Booster sessions may be needed to maintain results.
2. Is HIFEM suitable for severe UI?
HIFEM is highly effective for mild to moderate UI. Severe cases may require additional interventions.
3. Does HIFEM have any side effects?
The procedure is non-invasive and has no reported side effects.
4. Can I combine HIFEM with other treatments?
Yes, HIFEM can complement medications or exercises for enhanced results.
5. How soon will I see results?
Most patients notice improvements after a few sessions, with optimal outcomes evident by 6 months.